- ONCOLOGY Vol 16 No 9
- Volume 16
- Issue 9
Diagnosis and Management of Aplastic Anemia and Myelodysplastic Syndrome
The bone marrow failure states, aplastic anemia and myelodysplastic syndrome, are characterized by reticulocytopenic anemia, with variable neutropenia and thrombocytopenia. The bone marrow biopsy is very hypocellular in aplastic anemia, but it is usually hypercellular in myelodysplastic syndrome.
ABSTRACT: The bone marrow failure states, aplastic anemia and myelodysplastic syndrome, are characterized by reticulocytopenic anemia, with variable neutropenia and thrombocytopenia. The bone marrow biopsy is very hypocellular in aplastic anemia, but it is usually hypercellular in myelodysplastic syndrome. Marrow cytogenetic abnormalities are present in approximately half of myelodysplastic syndrome patients but are absent in aplastic anemia. Allogeneic bone marrow transplantation is the treatment of choice for young patients with severe aplastic anemia. Immunosuppressive therapy with antithymocyte globulin (ATG) and cyclosporine is used when transplantation is not the initial therapeutic choice; it induces responses in 65% to 80% of patients. Treatment of myelodysplastic syndrome is dependent upon risk classification, and patient age and performance status. Allogeneic stem cell transplantation should be considered for younger myelodysplastic syndrome patients. An acute myelogenous leukemia (AML) type of induction chemotherapy may benefit high-risk patients with a good performance status for whom allogeneic transplantation is not an option. Patients achieving a complete remission to induction chemotherapy may be considered for autologous stem cell transplantation. However, aggressive therapy is an option for only a minority of myelodysplastic syndrome patients; most receive supportive care. Anemia, and its related symptoms, is the principal problem for most myelodysplastic syndrome patients. Erythropoietin administration ameliorates anemia in a minority of myelodysplastic syndrome patients. A wide variety of novel experimental approaches including immunosuppressive therapy, angiogenesis inhibitors, platelet growth factors, and demethylating agents are now under investigation for myelodysplastic syndrome. [ONCOLOGY 16(Suppl 10):153-161, 2002]
Acquired aplastic anemia does not preferentially afflict any age group. Patients typically present with one or more symptoms related to pancytopenia. These may include fevers and chills, fatigue, dyspnea on exertion, mucosal bleeding, or petechial rash.
The peripheral blood counts usually are severely reduced, and the bone marrow biopsy is severely hypocellular. The remaining marrow elements usually consist of lymphocytes and plasma cells. Hypocellular myelodysplastic syndrome and hypocellular acute myeloid leukemia (AML) are excluded by performing flow cytometry and cytogenetics on the bone marrow. Increased numbers of myeloblasts or chromosomal abnormalities should not be observed in aplastic anemia.
In contrast to aplastic anemia, the incidence of myelodysplastic syndrome increases dramatically with age, and the majority of patients are elderly. They most commonly present with symptomatic anemia or incidentally noted peripheral blood abnormalities. Reticulocytopenic anemia is the most common laboratory abnormality; the red cells can be macrocytic, microcytic, or normocytic. Causes of megaloblastic anemia (vitamin B12 or folate deficiency) should be excluded when macrocytosis is present, and iron deficiency, anemia of chronic disease, or thalassemia minor should be considered in the setting of microcytosis.
Neutropenia and thrombocytopenia are variably present in myelodysplastic syndrome, but are more commonly associated with advanced disease. Thrombocytosis may occur in certain myelodysplastic syndrome subtypes, including those with an isolated 5q-cytogenetic abnormality or with increased numbers of ringed sideroblasts in the bone marrow.
The bone marrow biopsy is usually hypercellular for the patient’s age, although it is hypocellular in approximately 15% of cases. Erythroid dysplasia, including megaloblastic changes, binuclearity, or nuclear blebbing is a common feature of myelodysplastic syndrome. Ringed sideroblasts, abnormal erythroid precursors with iron-laden mitochondria ringing the nucleus, may be observed after Prussian blue staining.
Myeloid dysplasia may be characterized by increased numbers of immature forms (myeloid "left-shift"), or neutrophils with abnormal cytoplasmic granules or bilobed nuclei (pseudo-Pelger-Hut anomaly). Megakaryocytes may be abnormally small (micromegakaryocytes) or have abnormal nuclear morphology or ploidy. Increased numbers of bone marrow myeloblasts (> 5% of cellular elements) are present in more advanced myelo-dysplastic syndrome. Cytogenetics are abnormal in 50% to 60% of de novo cases of myelodysplastic syndrome and are useful in prognostication.
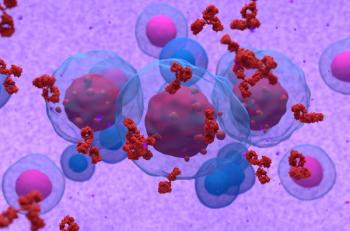
Although aplastic anemia and myelodysplastic syndrome are considered to be "bone marrow failure states" because of the defective production of mature peripheral blood cells, there are pathophysiologic differences between these two disorders.
The profound pancytopenia of aplastic anemia in association with the marked bone marrow hypocellularity suggests that there is a critical deficiency of hematopoietic progenitor cells. In most cases of acquired aplastic anemia, the hematopoietic progenitors are destroyed by autoreactive cytotoxic T lymphocytes.[1] The trigger for this autoimmune process cannot be identified in approximately three-quarters of patients. Known causes of aplastic anemia include various medications, rheumatologic disorders, hepatitis, pregnancy, and exposure to benzene.
The concurrence of peripheral blood cytopenias and bone marrow hypercellularity with an increase in immature precursors in myelodysplastic syndrome suggests that there is defective production of mature functional cells. Increasing evidence suggests that the common mechanism governing this process is intramedullary apoptosis. Locally increased levels of tumor necrosis factor-alpha or Fas ligand may induce hematopoietic progenitors to "commit suicide" by altering the normal intracellular ratio of antiapoptotic and proapoptotic proteins.[2,3] Alternatively, cytotoxic T lymphocytes may directly induce apoptosis of the abnormal hematopoietic progenitors.
It has long been appreciated that a number of cytogenetic abnormalities (especially 5q-,7q- or -7, +8, or 20q-) are characteristically observed in myelodysplastic syndrome.[4] The critical genes affected by these changes have not been identified, and therefore the mechanism of these cytogenetic defects on hematopoieis is unknown. The N-ras oncogene can be mutated in myelodysplastic syndrome, albeit infrequently, but this alteration may be of biological and clinical significance.[5]
TABLE 1
Classification of Aplastic Anemia
Patients with aplastic anemia are classified as having moderate, severe or very severe disease based on the number of lineages affected and the severity of the neutropenia (see Table 1). This classification is of prognostic significance for patients receiving medical therapy.[6,7] Bone marrow transplantation has typically been reserved for treatment of severe or very severe aplastic anemia.
TABLE 2
FAB Classification of Myelodysplastic Syndrome
The heterogeneity of myelodysplastic syndrome makes it a difficult disease to classify. The original French/American/British (FAB) classification was established to better characterize the morphologic features of myelodysplastic syndrome and to describe various subtypes.[8] Subsequently, this classification (see Table 2) was found to have prognostic value.[9] The prognostic scoring systems for myelodysplastic syndrome have been progressively refined.
TABLE 3
WHO Revision of the FAB Classification
The increasing availability of novel therapies for myelodysplastic syndrome requires accurate risk assessment for experimental subjects. One recent approach to improving prognostication in such patients is the World Health Organization (WHO) classification of myelodysplastic syndrome.[10] This refinement of the FAB classification subdivides the low-risk subtypes (refractory anemia [RA] and refractory anemia with ringed sideroblasts [RARS]) into very-low-risk groups, which have dysplasia of only the red cell lineage, and a higher-risk group, called refractory cytopenia with trilineage dysplasia (see Table 3).
In addition, the 5q- syndrome was identified as a unique subset of refractory anemia with an excellent prognosis. The intermediate-risk group, refractory anemia with excess of blasts (RAEB), was stratified into lower- and higher-risk groups based on the percentage of bone marrow blasts. The highest-risk group, refractory anemia with excess of blasts in transformation (RAEB-t), was reclassified as AML because patients with 20% to 30% bone marrow blasts have outcomes that are similar to those with > 30% blasts. Chronic myelomonocytic leukemia (CMML) was reclassified as a myeloproliferative disorder that may or may not have associated dysplastic features. This proposal remains controversial and requires further validation.
A perhaps more widely embraced prognostic tool is the International Prognostic Scoring System (IPSS).[11] This method assigns values to independent prognostic variables including percentage of bone marrow blasts, type of cytogenetic abnormality, and number of peripheral blood cytopenias, and generates a score that correlates with survival (see Tables 4 and 5). Many current clinical trials use this scoring system to establish enrollment criteria, or to stratify patients undergoing randomization.
Allogeneic Stem Cell Transplantation
TABLE 4
International Prognostic Scoring System for MDS TABLE 5
Survival and Risk of Leukemia for IPSS Risk Groups
The newly diagnosed aplastic anemia patient should be expeditiously assessed for the appropriateness of allogeneic stem cell transplantation and, if this is a suitable option, referred to a transplant center for treatment. Supportive care measures implemented prior to the transplant can significantly affect the outcome of the patient.
Unless there is an actively life-threatening requirement for transfusion of blood products, they should be absolutely minimized to prevent sensitization of the patient to alloantigens and minimize the risk of graft rejection. For the same reason, transfusion of blood products from family members must be prohibited.
All blood products should be seronegative for cytomegalovirus (CMV), leukocyte-reduced, and irradiated. The use of CMV-negative products should be continued unless the patient is seropositive for prior CMV exposure. Leukocyte reduction decreases the risk of allosensitization and decreases the risk of CMV transmission. Irradiation of blood products prevents the proliferation of alloreactive T lymphocytes that could potentially induce transfusion-related graft-vs-host disease (GVHD) in the patient posttransplant.
Allogeneic stem cell transplantation is appropriate as initial therapy for younger patients with severe aplastic anemia. Retrospective comparisons of allogeneic bone marrow transplantation (BMT) and immunosuppressive therapy for severe aplastic anemia have demonstrated a survival benefit of early transplantation in younger patients, although reports differ over whether age should be less than 20 years [12] or less than 40 years.[13]
Transplantation remains appropriate initial therapy for older patients, especially if very severe disease is present or if the patient has not received prior transfusions. An alternative strategy is to administer immunosuppressive therapy first and reserve transplantation for patients who do not respond to treatment.[14] Because immunosuppressive therapy takes several months to work, the principal risks of this approach relate to pancytopenia and allosensitization from the ongoing transfusion requirements.
The standard conditioning therapy prior to transplantation is cyclophosphamide (Cytoxan, Neosar) and antithymocyte globulin (ATG [Atgam]) for previously transfused patients, and cyclophosphamide alone for those who have not been transfused.[15,16] The survival following allogeneic BMT is 66% to 89% at 5 years.[16,17] Early risks of transplantation include graft failure (10%-15%), life-threatening (grade 3/4) acute GVHD (20%), and fatal infection or treatment-related organ failure (< 10%). Late risks include chronic GVHD (20%-40%) and late solid tumors (13%), especially squamous cell cancers.[18]
Immunosuppression with ATG and cyclosporine (Neoral, Sandimmune) is well established as standard therapy for aplastic anemia. Concurrent treatment with both drugs is significantly more effective than use of either drug alone.[19] The optimal duration of cyclosporine administration has not been evaluated systematically, but a minimum of 1 year of treatment, with gradual tapering over the subsequent year is recommended to minimize the risk of relapse. Renal function and transaminase levels should be monitored while patients are receiving cyclosporine and the drug dose should be adjusted if toxicity is observed.
The overall response to ATG/cyclosporine is 65% to 71% within 6 months of treatment. For patients achieving either a partial or complete response, survival is 57% after 10 years.[20-22] A randomized trial did not demonstrate a positive effect of granulocyte-colony stimulating factor (G-CSF, Neupogen), 5 µg/kg/d for 98 days, on the response rate or survival.[23]
The major risk of immunosuppressive therapy is fatal infection or bleeding (approximately 10%) from the underlying disease while awaiting a response. Other risks include disease relapse (35%-41%) and the development of acute myeloid leukemia or of myelodysplastic syndrome (10%-15% at 10 years).[20,22,24] Paroxysmal nocturnal hemoglobinuria can also occur as a late complication of aplastic anemia. Recently, high-dose cyclophosphamide without stem cell transplantation has been reported as an effective alternative immunosuppressive regimen with a high response rate (73%) and low risk of relapse.[25] However, preliminary data from a randomized trial comparing cyclophosphamide/cyclosporine to ATG/ cyclosporine found a higher rate of early death (20% vs 0%) for the cyclophosphamide group, but similar response rate (53% vs 81%) and relapse rate (25% vs 38%) for cyclophosphamide/cyclosporine compared to ATG/cyclosporine respectively.[26] Therefore, cyclophosphamide should be used for routine treatment of aplastic anemia.
Relapsed aplastic anemia can respond to a second course of ATG/cyclosporine or cyclosporine alone.[20] More than half of patients with relapsed aplastic anemia will respond to a second course of ATG.[24] "Cyclosporine dependence," defined as relapse associated with cyclosporine withdrawal, is fairly common and indicates the need to taper the cyclosporine dose very slowly over to 1 to 2 years, if possible.
Other Therapeutic Options
Therapeutic options for aplastic anemia that does not respond to an initial course of immunosuppression include unrelated donor stem cell transplantation or a second course of ATG. Because the survival following an unrelated transplant is best for patients who are transplanted within 1 year of diagnosis, the decision regarding this treatment is best made early.
Conditioning therapy requires total body irradiation in addition to cyclophosphamide/ATG in order to minimize the risk of graft rejection.[27] Improved survival 2 years after unrelated BMT has been reported for patients ≤ 20 years old (67%) compared to those > 20 years (43%) and for patients transplanted ≤ 1 year from diagnosis (73%), compared to 1 to 3 years (53%) or > 3 years (39%) after diagnosis.[27]
Single institutions have reported high response rates using horse ATG (64%) or rabbit ATG (77%) in patients who have not responded to an initial course of standard immunosuppressive therapy, but these numbers are perhaps double the results usually reported.[28,29] Nevertheless, a second course of ATG should be considered if no response is observed within 6 to 8 months after the initial treatment.
Prolonged cyclosporine administration as a single agent is occasionally effective. Hematopoietic growth factors, especially stem cell factor in combination with G-CSF, have induced trilineage responses in occasional refractory patients.[30] Chronic administration of a myeloid growth factor may be considered in patients with severe aplastic anemia and recurrent infections. A retrospective analysis showed no significantly increased risk of clonal hematologic disorders (myelodysplastic syndrome or AML) associated with G-CSF given for a median of 6 months.[31]
The heterogeneous nature of myelodysplastic syndrome makes the selection of appropriate therapy a potentially confounding process. The initial decision that should be made is whether a patient is an appropriate candidate for aggressive, potentially curative therapy, or instead should receive supportive care. The important clinical variables that contribute to this decision process include the patient’s age, performance status, disease prognosis, and the availability of a potential stem cell donor.
Allogeneic Stem Cell Transplantation
Allogeneic stem cell transplantation is a potentially curative option for myelodysplastic syndrome, but this therapy has traditionally been reserved for younger patients, who comprise only a small fraction of myelodysplastic syndrome patients. The selection of appropriate transplant candidates is complicated by the fact that low-risk patients, who could do well for several years with conservative management, have the best outcomes from transplantation, whereas high-risk patients do relatively poorly with each treatment strategy.
Allogeneic transplantation using related donors results in a 5-year relapse-free survival of 50% to 54% for myelodysplastic syndrome without increased bone marrow blasts and 31% to 36% for RAEB.[32,33] Survival is inversely related to the risk of relapse for each group, < 5% for myelodysplastic syndrome without increased blasts vs 50% with increased blasts. Other variables shown to affect survival posttransplant are the patient’s age, cytogenetic risk group, and time from diagnosis to transplant.[32-34]
Recently updated results of bone marrow transplantation using unrelated donors show that disease-free survival at 4 years was 26%. There was a high risk of treatment-related mortality (54%) due to infections, GVHD, and treatment-related toxicity. Clinical features associated with reduced risk of early mortality included younger age (< 20 years vs ³ 20 years), fully HLA-matched donor, and seronegativity for cytomegalovirus. In contrast to results using sibling donor, BMT using unrelated donors had a low risk of relapse (< 10%) for RA and RAEB subtypes.[35]
In an attempt to more successfully extend the use of allogeneic transplantation into older age groups, nonmyeloablative ("mini") transplants have been performed for a variety of hematologic disorders.[36,37] This treatment strategy involves the use of allogeneic cells primarily as immunotherapy against the malignant clone. The intensity of the conditioning chemotherapy is reduced in an attempt to minimize toxicity and the risk of GVHD. The conditioning therapy is principally immunosuppressive, and is intended to permit the engraftment of donor hematopoietic and immunoregulatory cells but not to eliminate the malignancy. Only a few myelodysplastic syndrome patients have been treated with this approach, but it will probably be best reserved for those at low risk, because the incidence of disease relapse for high-risk myelodysplastic syndrome will likely be higher with nonmyeloablative, compared to standard, conditioning therapy.
Autologous Stem Cell Transplantation
Autologous stem cell transplantation also is a potentially curable treatment for high-risk myelodysplastic syndrome. Following initial treatment with AML-type induction and consolidation chemotherapy, the autologous stem cells are collected. Standard high-dose conditioning therapy is then administered, followed by infusion of the autologous stem cells. This approach has produced a 40% disease-free survival rate 2 years posttransplant.[38] The potential advantage of autologous, compared to allogeneic, transplantation is that the risk of GVHD is avoided, but this is likely to be counterbalanced by a relatively high risk of disease relapse.
Chemotherapy
The effectiveness of chemotherapy for myelodysplastic syndrome has been extensively evaluated at M. D. Anderson Cancer Center.[39] Intensive chemotherapy regimens including various combinations of high-dose cytarabine, idarubicin (Idamycin), fludarabine (Fludara), and cyclophosphamide were evaluated sequentially in 394 patients with high-risk myelodysplastic syndrome over an 8-year period. Standard induction doses of cytarabine were not studied. Patients received one to two induction cycles followed by repeated cycles of the same chemotherapy drugs at reduced doses every 4 to 6 weeks for 6 to 24 months. The highest complete remission rate (72%) and longest median survival (88 weeks) were observed with the regimen containing high-dose cytarabine and idarubicin. This experience suggests that AML-type induction therapy can frequently induce remissions in high-risk myelodysplastic syndrome patients. A randomized comparison of consolidation chemotherapy vs autologous stem cell transplantation for high-risk myelodysplastic syndrome would be of interest.
Low-dose cytarabine has also been investigated as a potentially less toxic form of chemotherapy for myelodysplastic syndrome. Preliminary reports suggested that this treatment could induce remissions in patients with the illness, with acceptable side effects. However, a randomized trial comparing a 21-day cycle of low-dose cytarabine (10 mg/m2 bid) to supportive care showed that, in spite of a response rate of 32% in the chemotherapy arm, there was no significant difference in progression to AML or survival between the two groups.[40] Significantly more serious infections were observed in the treatment arm.
Interpretation of the study end points is confounded by the fact that 27% of the control patients were permitted to cross over to the treatment arm after 3 months. Nevertheless, in the absence of new data supporting low-dose cytarabine therapy, its use can only be recommended in a clinical trial setting.
Treatment of Anemia
The most common problem confronting patients with myelodysplastic syndrome is anemia and the associated fatigue. Transfusion support can provide only temporary relief from anemia-related symptoms, and the associated iron overload eventually necessitates chelation therapy.
Early trials of recombinant erythropoietin (Epogen, Procrit) in small numbers of myelodysplastic syndrome patients suggested that there was a potential therapeutic benefit from the drug. A meta-analysis reviewed the outcome of erythropoietin treatment in 205 patients enrolled in 17 trials and reported an overall response rate of 16%.[41] Interpretation of the results is complicated by the wide variety of drug doses and schedules used; in addition, one-third of the patients were treated using an intravenous route. Responses were more likely to occur in non-RARS than in RARS subtypes (21% vs 8%), in patients with a serum erythropoietin level < 200 U/L than in those with a level > 200 U/L (26% vs 10%), and in untransfused patients compared to transfused patients (44% vs 10%).
A randomized, double-blind, placebo-controlled trial of erythropoietin, 150 U/kg/d, demonstrated an erythroid response rate of 37% in treated patients compared to 11% for controls after 8 weeks.[42] These results clearly confirmed the activity of recombinant erythropoietin in myelodysplastic syndrome.
Trials have also evaluated the effects of combination therapy with erythropoietin and G-CSF in myelodysplastic syndrome. A Stanford study initiated erythropoietin at 100 U/kg/d subcutaneous (SC) and increased to 300 U/kg/d in the absence of response.[43] The G-CSF was started at 1 µg/kg/d SC and titrated to achieve either a normal neutrophil count, or twice the baseline level if it was normal initially. The red cell response in this trial was 48% and neutrophil response was 96%. The likelihood of response was higher when the baseline erythropoietin level was < 500 U/L than when it was > 500 U/L (65% vs 20%).
TABLE 6
NCCN Recommendations for Treating Anemia in MDS
Based on the available data, the National Comprehensive Cancer Network (NCCN) published guidelines in 1998 for the treatment of anemia in myelodysplastic syndrome (see Table 6).[44] For initial treatment of non-RARS myelodysplastic syndrome patients with a serum erythropoietin level < 500 U/L, the recommended dose of erythropoietin was 150 to 300 U/kg/d SC. For nonresponders, or patients with RARS, the NCCN recommended adding G-CSF, 0.3 to 3 µg/kg/d, to the erythropoietin regimen. It should be noted, however, that the regimen of erythropoietin plus G-CSF has not been compared to erythropoietin alone in a prospective, randomized clinical trial.
Daily erythropoietin administration has been largely supplanted in clinical practice by thrice-weekly 10,000 U dosing, with transition to a single dose of 40,000 U/wk for responding patients. Unfortunately, there are no clinical trials comparing the efficacy of these various dosing regimens.
Treatment of Neutropenia
Myeloid growth factors have been evaluated as therapy for the neutropenia experienced by many patients with myelodysplastic syndrome. Although the majority of such patients experience a neutrophil response to G-CSF or granulocyte-macrophage colony-stimulating factor (GM-CSF, Leukine), the clinical benefit of these responses is unproved.
A phase III randomized clinical trial compared G-CSF, 0.5-10 µg/kg/d, to supportive care in 102 patients with either RAEB or RAEB-t.[45] Unexpectedly, the RAEB patients treated with G-CSF had significantly reduced survival compared to the control arm (10 vs 21 months). The RAEB-t patients had similar outcomes in both arms. There was no difference in the rate of AML evolution between the treatment and control groups. Although retrospective review of the treatment assignment using the IPSS revealed that more high-risk RAEB patients were enrolled in the treatment arm than in the control arm, chronic myeloid growth factor support is not recommended for routine prophylaxis of neutropenia in myelodysplastic syndrome.
Novel Approaches
Novel approaches to therapy have evolved in the last few years to include immunosuppressive therapy, antiapoptotic regimens, novel hematopoietic growth factors, demethylating agents, platelet growth factors, and other agents.
TABLE 7
ATG Protocol for Aplastic Anemia
Although ATG was first used in aplastic anemia more than 20 years ago, it has only recently been evaluated in myelodysplastic syndrome patients. A National Institutes of Health study treated 61 red cell transfusion-dependent patients with RA, RARS, or RAEB using a standard ATG protocol (see Table 7).[46,47] Transfusion independence was achieved in 31% of patients within 8 months of treatment. Responses were more frequent in patients with RA than in those with RAEB or RARS. Hemoglobin responses were stable in 81% of patients. In addition, responding patients were noted to have concomitant improvements in neutrophil or platelet counts. The high rate of stable response suggests a previously unappreciated role for T lymphocytes in mediating the intramedullary apoptosis of hematopoietic progenitors in myelodysplastic syndrome.
Thalidomide (Thalomid) is another old drug that has recently been applied therapeutically in myelodysplastic syndrome.[48] Thalidomide inhibits apoptosis induced by tumor necrosis factor-alpha and has antiangiogenic activity. Thalidomide was administered at doses of 100 to 400 mg daily to 83 myelodysplastic syndrome patients for 12 weeks. Of the patients completing the planned therapy, 31% had an erythroid response. Overall, 17% of the patients failed to complete the 12-week course due to drug toxicity including fatigue, constipation, shortness of breath, fluid retention, dizziness, rash, or peripheral neuropathy. The efficacy of thalidomide in myelodysplastic syndrome is currently being evaluated in a phase III trial.
5-Aza-2´-deoxycytidine (decitabine) is a DNA methylation inhibitor that may be capable of inducing the expression of genes that can reverse the blockade to cellular differentiation observed in myelodysplastic syndrome. Treatment with decitabine, 45 mg/m2/d for 3 days every 6 weeks, was administered to 66 myelodysplastic syndrome patients.[49] The overall response rate was 49%, but 64% of patients with IPSS high-risk disease responded and 31% had major cytogenetic responses after a median of three treatment cycles.[50] Grade 3/4 toxicities included peripheral blood cytopenias, fever, and infection. Decitabine is currently undergoing phase III evaluation for the treatment of myelodysplastic syndrome.
Amifostine (Ethyol), a free-radical-scavenging agent approved to ameliorate cisplatin-induced renal toxicity, was incidentally noted to stimulate hematopoiesis in vitro. Subsequently, 117 patients with myelodysplastic syndrome were treated with amifostine, 200 or 400 mg/m2 thrice weekly for 3 weeks, followed by 2 weeks of rest.[51] Of the 75 patients evaluable for response, 36% had improvement in one or more peripheral blood lineages, and 20% of the red cell transfusion-dependent patients had at least a 50% decrease in transfusion requirements. However, the median response duration was short (41 days), and continued response required chronic treatment. Side effects were moderate, with grade 3 toxicities including fatigue (18%), nausea (36%), and vomiting (27%). These difficulties are likely to limit the clinical utility of this drug in myelodysplastic syndrome.
Two recombinant human platelet growth factors are clinically available, interleukin (IL)-11 and thrombopoietin, but so far, there has been only limited clinical experience with IL-11 in myelodysplastic syndrome. Two small studies suggested that IL-11, given subcutaneously at doses of 10 µg/kg/d or 5,000 µg once weekly could improve the platelet counts of approximately half of thrombocytopenic patients with myelodysplastic syndrome.[52,53] Only mild side effects were reported. Unfortunately, myelodysplastic syndrome patients with severe thrombocytopenia usually have advanced disease and a high risk of AML progression, which would not be favorably affected by platelet growth factors.
It is encouraging that the number of new therapies for myelodysplastic syndrome has increased rapidly in recent years. As more is learned about the pathogenesis of this group of disorders, it is likely that specific, targeted therapies will become available to treat myelodysplastic syndrome subtypes that share common molecular abnormalities. The enrollment of appropriate patients into clinical trials is strongly encouraged, in order to expedite the evaluation of promising new therapies for myelodysplastic syndrome.
References:
1. Young N, Maciejewski J: The pathophysiology of acquiredaplastic anemia. N Engl J Med 336(6):1365-1372, 1997.
2. Gersuk GM, Beckham C, Loken MR, et al: A role for tumournecrosis factor-a,Fas and Fas-ligand in marrow failure associated with myelodysplastic syndrome. BrJ Haematol 103:176-188, 1998.
3. Parker JE, Fishlock KL, Czepulkowski MB, et al: "Lowrisk" myelodysplastic syndrome is associated with excessive apoptosis andan increased ratio of pro- versus anti-apoptotic bcl-2-related proteins. Br JHaematol 103:1075-1082, 1998.
4. Fenaux P, Morel P, Lai JL: Cytogenetics of myelodysplasticsyndromes. Semin Hematol 33(2):127-138, 1996.
5. Paquette RL, Landaw EM, Pierre RV, et al: N-ras mutationsare associated with poor prognosis and increased risk of leukemia inmyelodysplastic syndrome. Blood 82(2):590-599, 1993.
6. Marsh JCW, Hows JM, Bryett KA, et al: Survival afterantilymphocyte globulin therapy for aplastic anemia depends on disease severity.Blood 70:1046-1052, 1987.
7. Paquette RL, Tebyani N, Frane M, et al: Long-term outcomeof aplastic anemia in adults treated with antithymocyte globulin: Comparisonwith bone marrow transplantation. Blood 85(1):283-290, 1995.
8. Bennet JM, Catovsky D, Daniel MT, et al: Proposals for theclassification of the myelodysplastic syndromes. Br J Haematol51:189-199, 1982.
9. Mufti GJ, Stevens JR, Oscier DG, et al: Myelodysplasticsyndromes: A scoring system with prognostic significance. Br J Haematol59:425-433, 1985.
10. Harris NL, Jaffe ES, Diebold J, et al: World HealthOrganization Classification of neoplastic diseases of the hematopoietic andlymphoid tissues: Report of the Clinical Advisory Committee Meeting, AirlieHouse, Virginia, November 1997. J Clin Oncol 17(12): 3835-3849, 1999.
11. Greenberg P, Cox C, LeBeau MM, et al: Internationalscoring system for evaluating prognosis in myelodysplastic syndromes. Blood89:2079-2088, 1997.
12. Bacigalupo A, Hows J, Wursch A, et al: Treatment ofsevere aplastic anemia(AA) with bone marrow transplantation (BMT) orimmunosuppression: A report of the EBMT SAA Working Party, in Aplastic Anemiaand Other Bone Marrow Failure Syndromes, pp 115-120. New York, Springer-Verlag,1989.
13. Doney K, Leisenring W, Storb R, et al: Primary treatmentof acquired aplastic anemia: Outcomes with bone marrow transplantation andimmunosuppressive therapy. Ann Intern Med 126:107-115, 1997.
14. Crump M, Larratt LM, Maki E, et al: Treatment of adultswith severe aplastic anemia: Primary therapy with antithymocyte globulin (ATG)and rescue of ATG failures with bone marrow transplantation. Am J Med92:596-602, 1992.
15. Anasetti C, Doney KC, Storb R, et al: Marrowtransplantation for severe aplastic anemia. Ann Intern Med 104:461-466,1986.
16. Storb R, Anasetti ER, Appelbaum FR, et al: Long-termfollow-up of allogeneic marrow transplantation in patients with aplastic anemiaconditioned by cyclophosphamide combined with antithymocyte globulin (letter). Blood89:3890-3891, 1997.
17. Passweg JR, Socié G, Hinterberger W, et al: Bone marrowtransplantation for severe aplastic anemia: Has outcome improved? Blood90(2):858-864, 1997.
18. Deeg HJ, Socié G, Schoch G, et al: Malignancies aftermarrow transplantation for aplastic anemia and Fanconi anemia: A joint Seattleand Paris analysis of results in 700 patients. Blood 87(1):386-392, 1996.
19. Frickhofen N, Kaltwasser JP, Schrezenmeier H, et al:Treatment of aplastic anemia with antilymphocyte globulin and methylprednisolonewith or without cyclosporine. N Engl J Med 324(19):1297-1304, 1991.
20. Rosenfeld SJ, Kimball J, Vining D, et al: Intensiveimmunosuppression with antithymocyte globulin and cyclosporine as treatment forsevere aplastic anemia. Blood 85(11):3058-3065, 1995.
21. Bacigalupo A, Bruno B, Saracco P, et al: Antilymphocyteglobulin, cyclosporine, prednisolone, and granulocyte colony-stimulating factorfor severe aplastic anemia: An update of the GITMO/EBMT study on 100 patients. Blood95(6):1931-1934, 2000.
22. Frickhofen N, Kaltwasser JP, Heimpel H, et al: 10 yearsresults of a German phase III trial evaluating treatment of aplastic anemia withantithymocyte globulin with or without cyclosporine A. Blood 94(10 suppl1):674a, 1999.
23. Gluckman E, Rokicka-Milewska R, Gordon-Smith EC, et al:Results of a randomized study of glycosylated rHuG-CSF lenograstim in severeaplastic anemia. Blood 92(10 suppl 1):376a, 1998.
24. Shrezenmeier H, Marin P, Raghavachar A, et al: Relapse ofaplastic anemia after immunosuppressive treatment: A report from the EuropeanBone Marrow Transplantation Group SAA Working Group. Br J Haematol85:371-377, 1993.
25. Brodsky RA, Sensenbrenner LL, Smith BD, et al: Durabletreatment-free remission after high-dose cyclophosphamide therapy for previouslyuntreated severe aplastic anemia. Ann Intern Med 135:477-483, 2001.
26. Tisdale JF, Maciejewski JP, Nunez O, et al: A randomizedtrial comparing antithymocyte globulin and cyclosporine to cyclophosphamide andcyclosporine for initial treatment in severe aplastic anemia: results oflong-term follow-up. Blood 98(11 suppl 1):223a, 2001.
27. Deeg HJ, Amylon MD, Harris RE, et al: Marrow transplantsfrom unrelated donors for patients with aplastic anemia: Minimum effective doseof total body irradiation. Biol Blood Marrow Transplantation 7:208-215,2001.
28. Tichelli A, Passweg J, Nissen C, et al: Repeatedtreatment with horse antilymphocyte globulin for severe aplastic anemia. Br JHaematol 100:393-400, 1998.
29. Di Bona E, Rodeghiero F, Bruno B, et al: Rabbitantithymocyte globulin (r-ATG) plus cyclosporine and granulocyte colonystimulating factor is an effective treatment for aplastic anaemia patientsunresponsive to a first course of intensive immunosuppressive therapy. Br JHaematol 107:330-334, 1999.
30. Kurzrock R, Paquette R, Gratwohl A, et al: Use of stemcell factor (Stemgen, SCF) and filgrastim (G-CSF) in aplastic anemia patientswho have failed ATG/ALG therapy. Blood 90(10 suppl 1):173a, 1997.
31. Locasciulli A, Arcese W, Locatelli F, et al: Treatment ofaplastic anaemia with granulocyte-colony stimulating factor and risk ofmalignancy. Lancet 357:43-44, 2001.
32. Anderson JE, Appelbaum FR, Storb R: An update onallogeneic marrow transplantation for myelodysplastic syndrome. LeukemiaLymphoma 17:95-99, 1995.
33. Sutton L, Chastang C, Ribaud P, et al: Factorsinfluencing outcome in de novo myelodysplastic syndromes treated by allogeneicbone marrow transplantation: A long-term study of 71 patients. Blood88(1):358-365, 1996.
34. Nevill TJ, Fung HC, Shepherd JD, et al: Cytogeneticabnormalities in primary myelodysplastic syndrome are highly predictive ofoutcome after allogeneic bone marrow transplantation. Blood92(6):1910-1917, 1998.
35. Castro-Malaspina H, Harris RE, Gajewski J, et al:Unrelated donor marrow transplantation for myelodysplastic syndromes: Outcomeanalysis in 510 transplants facilitated by the National Marrow Donor Program. Blood99(6):1943-1951, 2002.
36. Slavin S, Nagler A, Naparstek E, et al: Nonmyeloablativestem cell transplantation and cell therapy as an alternative to conventionalbone marrow transplantation with lethal cytoreduction for the treatment ofmalignant and nonmalignant hematologic disorders. Blood 91(3):756-763,1998.
37. Khouri IF, Keating M, Körbling M, et al: Transplant-lite:Induction of graft-versus-malignancy using fludarabine-based nonablativechemotherapy and allogeneic blood progenitor-cell transplantation as treatmentfor lymphoid malignancies. J Clin Oncol 16(8):2817-2824, 1998.
38. de Witte T: Stem cell transplantation in myelodysplasticsyndromes. Forum Trends Exp Clin Med 9:75-81, 1999.
39. Beran M, Shen Y, Kantarjian H: High-dose chemotherapy inhigh-risk myelodysplastic syndrome. Cancer 92:1999-2015, 2001.
40. Miller KB, Kyungmann K, Morrison FS, et al: Theevaluation of low-dose cytarabine in the treatment of myelodysplastic syndromes:A phase-III intergroup study. Ann Hematol 65:162-168, 1992.
41. Hellström-Lindberg E: Efficacy of erythropoietin in themyelodysplastic syndromes: A meta-analysis of 205 patients from 17 studies. BrJ Haematol 89:67-71, 1995.
42. Italian Cooperative Study Group for rHuEpo inMyelodysplastic Syndromes: A randomized double-blind placebo-controlled studywith subcutaneous recombinant human erythropoietin in patients with low-riskmyelodysplastic syndrome. Br J Haematol 103:1070-
1074, 1998.
43. Negrin RS, Stein R, Doherty K, et al: Maintenancetreatment of the anemia of myelodysplastic syndromes with recombinant humangranulocyte colony-stimulating factor and erythropoietin: Evidence for in vivosynergy. Blood 87(10):4076-4081, 1996.
44. National Comprehensive Cancer Network: NCCN practiceguidelines for the myelodysplastic syndromes. Oncology 12(11A):53-
80, 1998.
45. Greenberg P, Taylor K, Larson R et al: Phase IIIrandomized multicenter trial of G-CSF vs observation for myelodysplasticsyndromes (MDS). Blood 82(10 suppl 1):196a, 1993.
46. Molldrem JJ, Caples M, Mavroudis D, et al: Antithymocyteglobulin for patients with myelodysplastic syndrome. Br J Haematol99:699-705, 1997.
47. Molldrem JJ, Leifer E, Bahcece E, et al: Antithymocyteglobulin for treatment of the bone marrow failure associated withmyelodysplastic syndromes. Ann Intern Med 137(3):156-163, 2002.
48. Raza A, Meyet P, Dutt D, et al: Thalidomide producestransfusion independence in long-standing refractory anemias of patients withmyelodysplastic syndromes. Blood 98(4):958-965, 2001.
49. Wijermans P, Lübbert M, Verhoef G, et al: Low-dose5-aza-2´-deoxycytidine, a DNA hypomethylating agent, for the treatment ofhigh-risk myelodysplastic syndrome: A multicenter phase II study in elderlypatients. J Clin Oncol 18(5):956-962, 2000.
50. Lübbert M, Wijermans P, Kunzmann R, et al: Cytogeneticresponses in high-risk myelodysplastic syndrome following low-dose treatmentwith the DNA methylation inhibitor 5-aza-2´-deoxycytidine. Br J Haematol114: 349-357, 2001.
51. List AF, Brasfield F, Heaton R, et al: Stimulation ofhematopoiesis by amifostine in patients with myelodysplastic syndrome. Blood90(9):3364-3369, 1997.
52. Kurzrock R, Cortes J, Thomas D, et al: Low doseinterleukin-11 is well-tolerated and induces platelet responses inmyelodysplasia and other bone marrow failure states. Blood 96(11):147a,2000.
53. Case DC: Weekly low dose interleukin-11 in myelodysplasia. Blood 98(11):624a, 2001.
Â
Articles in this issue
over 23 years ago
The Molecular Basis of Cancer, 2nd Editionover 23 years ago
Management of Anemia in Patients With Cancerover 23 years ago
Commonly Used Quality of Life and Symptom Measurement Scalesover 23 years ago
Iron and the Anemia of Chronic Diseaseover 23 years ago
Recombinant Human Erythropoietin in Cancer-Related Anemiaover 23 years ago
When Is it Justified to Treat Symptoms? Measuring Symptom Burdenover 23 years ago
Overcoming Barriers to Erythropoietic TherapyNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.