Oncology NEWS International
- Oncology NEWS International Vol 15 No 6
- Volume 15
- Issue 6
FDA Approves Dacogen for Treating All MDS Subtypes
The Food and Drug Administration (FDA) has approved the marketing of Dacogen (decitabine for injection, MGI Pharma) for the treatment of all forms of myelodysplastic syndrome (MDS). The agency acted after reviewing data submitted by the sponsor from a pivotal phase III trial, in which patients evaluable for response had a 21% overall response rate, and two supporting studies.
ROCKVILLE, MarylandThe Food and Drug Administration (FDA) has approved the marketing of Dacogen (decitabine for injection, MGI Pharma) for the treatment of all forms of myelodysplastic syndrome (MDS). The agency acted after reviewing data submitted by the sponsor from a pivotal phase III trial, in which patients evaluable for response had a 21% overall response rate, and two supporting studies.
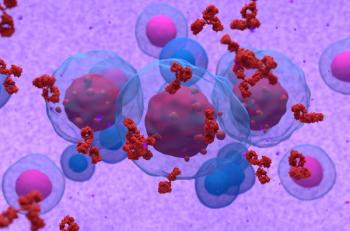
MDS consists of a group of disorders in which a person's bone marrow produces poorly functioning and immature cells. Physicians diagnose an estimated 7,000 to 12,000 new cases annually in the United States, according to the FDA, with the highest prevalence in people age 60 and older. MDS may develop after a patient undergoes drug or radiation treatments, but often the cause goes undetermined. Some MDS patients require chronic blood transfusions and some forms of the disease progress to acute myeloid leukemia (AML).
"Dacogen represents a new treatment option that can reduce or eliminate the need for patients with MDS to receive frequent blood transfusions, which is an important clinical benefit," said Hagop Kantarjian, MD, of M.D. Anderson Cancer Center and clinical investigator of the ongoing Dacogen clinical development program for MDS and AML. "This approval is a major advance in our fight against myelodysplastic syndromes." The FDA-approved indication for Dacogen includes previously treated and untreated, de novo, and secondary MDS of all French-American-British (FAB) subtypes and intermediate-1, intermediate-2, and High-Risk International Prognosis Scoring System (IPSS) groups.
MGI Pharma expects to make the drug commercially available no later than the end of June. "We look forward to providing clinicians with an effective therapy to offer their MDS patients," said Lonnie Moulder, the company's president and CEO. "MGI Pharma is committed to continuing the development of Dacogen for patients with AML, chronic myelogenous leukemia, and solid tumors, in addition to developing alternative dosing regiments for patients with MDS."
Dacogen is a new molecular entity given orphan drug status by FDA. The drug appears to exert its antineoplastic action after phosphorylation and direct incorporation into DNA. This activity leads to inhibition of the enzyme methyltransferase and results in cellular differentiation or cell death. The drug was originally developed and its clinical testing supported by SuperGen Corp., which acquires, develops, and commercializes oncologic and hematologic therapies.
Pivotal Study
The phase III pivotal study presented by the sponsor was a randomized, open-label, multicenter, controlled study. It involved 170 adults with MDS forms meeting FAB criteria and IPSS High Risk, intermediate-1, and intermediate-2 prognostic scores. Researchers randomized 89 patients to Dacogen plus supportive care (83 of whom received the drug) and 81 to supportive care alone. Patient mean age was 69 in the treatment arm and 67 in the control group. Patients received the drug by IV infusion, 15 mg/m2 over a 3-hour period every 8th hour for 3 consecutive days. This therapy was repeated every 6 weeks, and patients underwent a median of three Dacogen cycles.
Study protocol excluded patients with AML. However, an independent review found that nine patients in the treatment arm and three in the supportive-care group had a diagnosis of AML at baseline. Some of the AML patients who received Dacogen experienced responses.
The primary trial endpoints were overall response rate and time to AML or death. Response results were based on 89 patients in the intent-to-treat group. Secondary endpoints included duration of response and hematologic improvement.
Fifteen (17%) of the 89 patients in the intent-to-treat Dacogen arm demonstrated a response; 8 (9%) had a complete response and 7 (8%) a partial response. All but one of these patients responded by the fourth cycle. However, among the 56 Dacogen-treated patients considered evaluable for responsethose who had confirmed MDS at baseline and who received at least two cycles of treatmentthe overall response rate was 21%.
No one in the supportive-care arm showed a response. Researchers found no significant difference in mean time to AML or death between the Dacogen-treated patients and those who received supportive care.
In the intent-to-treat Dacogen patients, the median time to achieving a complete or partial response was 93 days (range, 55 to 272 days). The median duration of response was 288 days (range, 116 to 388 days). Those patients who had a response required no transfusions during its duration.
Benefit was observed in an additional 13% of the Dacogen group in the form of hematologic improvement, compared to 7% in the supportive-care arm. Improvement was defined as less than a partial response that lasted at least 8 weeks.
The two supportive studiesboth open-label, single-arm, multicenter trials conducted in Europe and open to any FAB subtypeinvolved a total of 164 patients. The results of these studies proved consistent with the phase III trial, with overall response rates of 26% and 24%.
The highest incidence of grade 3 or 4 events in the Dacogen arm of the pivotal trial included neutropenia (87%), thrombocytopenia (85%), febrile neutropenia (23%), and leukopenia (22%). Eight of the 83 patients treated with Dacogen permanently discontinued therapy because of adverse events, compared to one patient in the supportive-care arm.
In the three studies, researchers found no overall safety difference between patients older or younger than age 65, nor did the studies show a significant difference in safety or efficacy by sex.
Articles in this issue
over 19 years ago
Triple-Negative Cancers More Common in Young Black Ptsover 19 years ago
Artists Turn Flowers & Curves Into 'Forms' and 'Figures'over 19 years ago
Study to Examine Outcomes Disparities in Pediatric ALLover 19 years ago
Thalidomide Has 'Changed the Paradigm' in Myeloma Rxover 19 years ago
CA4P Gets Orphan Drug Statusover 19 years ago
Testicular Ca Survivors at Increased Risk for CV Eventsover 19 years ago
A Novel Brings a Cancer Research Laboratory to Lifeover 19 years ago
NCCN Reveals New Venous Thromboembolism Guidelineover 19 years ago
Lapatinib New Option for Metastatic HER2+ Breast Caover 19 years ago
Noninvasive Ablation Relieves Chronic Chest Wall PainNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.