Oncology NEWS Today Blog
- Oncology NEWS Today Blog Vol 18 No 11
- Volume 18
- Issue 11
Making the most of gastric imaging requires clear communication between oncologists and radiologist
There is a complex array of tests for imaging the abdomen, but there are really only three things that oncologists need to tell radiologists in order to get the most from these imaging studies, according to Fergus V. Coakley, MD, chief of abdominal imaging at the University of California, San Francisco. “We need you to tell us the working diagnosis; what treatment the patient has had; and, the most critical, what is the question you want answered by this test? That’s the most important one,” Dr. Coakley said during a presentation at ASCO 2009 in Orlando.
There is a complex array of tests for imaging the abdomen, but there are really only three things that oncologists need to tell radiologists in order to get the most from these imaging studies, according to Fergus V. Coakley, MD, chief of abdominal imaging at the University of California, San Francisco. “We need you to tell us the working diagnosis; what treatment the patient has had; and, the most critical, what is the question you want answered by this test? That’s the most important one,” Dr. Coakley said during a presentation at ASCO 2009 in Orlando.
“Is it to confirm the diagnosis? Evaluate the patient for surgery? Evaluate response to therapy? All of these things will influence the choice of the test, how we do it, and how we interpret it,” Dr. Coakley said at the education session jointly sponsored by ASCO and RSNA.
This exchange of clinical information between oncologist and radiologist is critical to achieve the best patient care, added Dr. Coakley, who is also a professor of radiology and urology and vice chair of clinical services at UCSF. “We need to talk to each other. It is going to improve how you pick your tests, how they are performed, and how they are interpreted,” he said.
Choice of test
PET/CT is a good test for evaluating extent of disease in patients who are surgical candidates. Dr. Coakley described the case of a 30-year-old woman with familial adenomatous polyposis who had undergone sigmoidectomy two months earlier for node-negative colon cancer. She had a new liver metastasis detected on CT and surgery was being considered.
This patient was a candidate for whole-body PET/CT to see whether there was extrahepatic disease, he said. Indeed, her scan showed that she actually had two extrahepatic sites of metastatic disease, which made her ineligible for surgery. “This is a prime example of how whole-body PET/CT can really help you fully evaluate the true extent of disease in these presurgical patients,” he said.
A baseline PET scan can also be useful in pretreatment patients. Dr. Coakley discussed a patient with metastatic breast cancer in whom a new sclerotic focus in the spine (L1) developed. Most clinicians would assume that this was a progression of disease, he said, but in fact, the baseline PET scan showed metastasis that was occult on a CT scan.
“This is an example of healing by sclerosis and pseudoprogression, and is a good example of how a baseline PET can help you. I’m not sure you need to follow up these patients with PET, but I think a baseline PET gives you the best single-shot evaluation of disease extent,” he said.
It’s also important to know which tests are not appropriate given the circumstances. For instance, PET has low sensitivity for brain metastases, so gadolinium-enhanced MRI may be a better option. PET also has low sensitivity for mucinous colorectal cancer.
“PET may also be negative after treatment,” Dr. Coakley said. “Oncologists tend to regard that as a false-negative but that’s debatable and the issue may be one of terminology. Maybe you have actually suppressed that tumor metabolically, but you may still have measureable, residual disease on CT and have a totally negative PET scan.”
Finally, PET/CT should always be done with contrast. “It is an abomination to do an expensive PET scan and then link it to a dull, dark CT scan and to call that a non-diagnostic CT,” Dr. Coakley said. However, there is a sizeable radiation dose associated with CT, which makes it less suitable in certain patients, such as younger patients with low-risk testicular cancer or lymphoma, he added.
Test technique
Once the appropriate test has been agreed on, the technique must be decided on as well. Dr. Coakley cited an example of a 45-year-old patient with cirrhosis and a rising alpha-fetoprotein level. Would a standard portal venous phase CT scan be enough? Not in this case, “because hepatocellular carcinoma is one of those tumors that is often hypervascular and seen best on the arterial phase. One of the big questions when we do a CT scan is: are we going to do single-phase or multi-phase? Most of the time, the single portal venous phase is perfectly adequate because most tumors are hypovascular,” he said.
As with hepatocellular carcinoma, there are some tumors that are hypervascular and can only be seen on the arterial phase, such as neuroendrocrine metastases.
Test interpretation
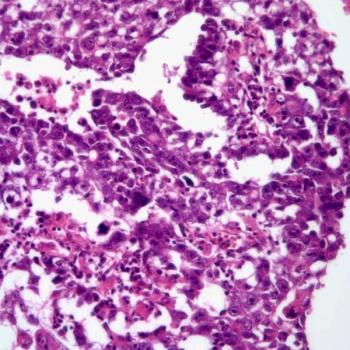
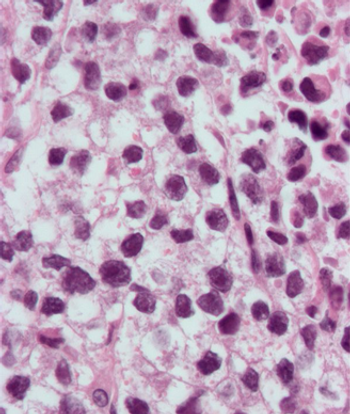
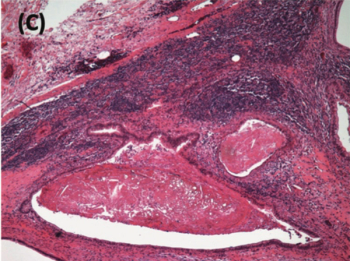
Dr. Coakley illustrated the importance of providing a complete clinical history to the radiologist with the case of a 64-year-old woman with breast cancer. On the basis of imaging studies, the report came back as a large breast mass with axillary and abdominal adenopathy, consistent with breast cancer and nodal metastases (see Figures 1-3).
“On the face of it, that interpretation was justifiable, until you get the extra information: she was two months’ postsurgery so the breast and axillary changes were likely postoperative,” he said. “She had a negative PET for those nodes in the abdomen (see Figure 4). She had hepatitis C and we often see reactive nodes in that setting, so probably those abdominal nodes were reactive and not metastatic. All that missing information totally changes the interpretation.”
Clinical information imparted by the oncologist helps the radiologist be a better diagnostician, which ultimately optimizes patient care. “We really need to have all of the clinical information as well as the previous radiological history and imaging tests,” Dr. Coakely said. “How you achieve that communication will depend a little bit on local practice, but I really think that developing personal relationships with your radiologist is very important. I work very closely with our oncologists and gastrointestinal and genitourinary oncologists at UCSF, and I think that really does improve patient care.”
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.