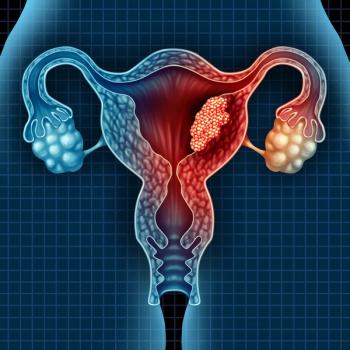
Molecular Profiling and Risk Stratification in Advanced Endometrial Carcinoma
David O’Malley, MD, an expert gynecologic oncologist, details molecular profiling and risk stratification for patients with advanced endometrial carcinoma.
Episodes in this series
Transcript:
David M. O’Malley, MD: There are what we classically defined as low-risk and high-risk histological subtypes are type 1 and type 2. We really have gotten much smarter. Endometrioid, which is the most common, meaning that more than 80% of uterine cancers in general are either grade 1, 2, or 3. We’ve also actually gone to a 2-grade system, low versus high. You also have higher risk histology, a higher chance of recurring, which includes the serous cancer of the uterus, clear cell, [and] carcinosarcoma, which are not really a sarcoma but an epithelial tumor with sarcoma components, but it’s the epithelial component that drives its behavior usually. We also have rare histology called mucinous. But really, it’s endometrioid grades 1 to 3, serous [and] clear cell, and carcinosarcoma. Now, the histologies are very important.
We actually saw a presentation at this year’s SGO [Society of Gynecologic Oncology] by Dr Alex Olawaiye that the guidelines are going to change for FIGO [The International Federation of Gynecology and Obstetrics] and they’re actually going to incorporate molecular staging. There are 4 main types of molecular tumors: POLE [polymerase] ultramutated, MSI [microsatellite instability] high hypermutated, copy number low, [and] copy number high. Now, the POLE hypermutated, need to have next-generation sequence or at least spot mutation analysis in order to identify those patients, and that’s only about 4% of endometrial cancers. The hypermutated are those loss of MMR [mismatch repair] deficient patients. More MMR loss of MMR proteins. The copy number high has all their mismatch repair proteins present, and those are the endometrioid cancers usually. And then the copy number high, those are usually p53 mutated or abnormal. It only represents about 10% of our uterine cancers. But actually, the worst prognosis is high as 30% to 40% of our overall recurrences. And when we look at these, we are now moving. Everybody should have, obviously, still the histology; mismatched repair deficiency testing, or protein testing with IHC [immunohistochemistry]; probably need to have ER, estrogen receptor, at this point. And then identifying workflows to identify those patients with POLE mutations.
We talked about [how] the stage is going to really completely change to bring in molecular staging. So all these patients, you’re going to need to know the molecular makeup of these tumors. When we look at the early-stage disease, which are really going to be the endometrioids confined to the uterus. But actually, the new staging system, anybody with a high-risk histology or p53 mutated or not normal is actually going to be considered stage 2, and this is new, this is completely new. In our staging, typically, we identify those as stage 1 knowing that [there is] a high recurrence rate and treat them with systemic therapy. Advanced-stage disease, metastatic to the fallopian tube, metastatic to the lymph nodes, but referred to as local-regional disease, will continue to be present. But one changes if there’s just disease in the pelvic peritoneum. They’re now calling that stage 3, and previously this was called stage 4. Again, I’m not sure there’s a magic window separating the pelvic peritoneum from the upper abdominal peritoneum. But the staging has changed [to] reflect that if somebody has metastatic disease, visceral mass or intra-abdominal mass, even to the omentum, it’s still considered stage 4. So we still utilize those stages but the molecular signature is going to be key. Now and even more so in the future with regards to treatment [INAUDIBLE] of endometrial cancer.
Transcript edited for clarity.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.