A Step Forward for Targeted Agents in Advanced NETs?
Lenvatinib offers the highest published response rate to a targeted agent for patients with advanced neuroendocrine tumors, but the agent’s precise role in this setting remains in question.
A phase II trial showed that lenvatinib offered the highest published response rate to a targeted agent for patients with advanced neuroendocrine tumors (NETs). The agent’s precise role in this setting remains in question.
“Patients with advanced NETs have limited treatment options,” said Jaume Capdevila, MD, of Vall d’Hebron Institute of Oncology in Barcelona, during his presentation at the European Society for Medical Oncology (ESMO) 2018 Congress. A number of agents are approved for these patients, but response rates with many of them are below 5%.
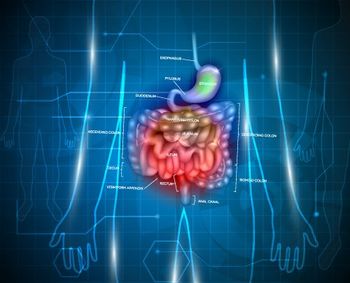
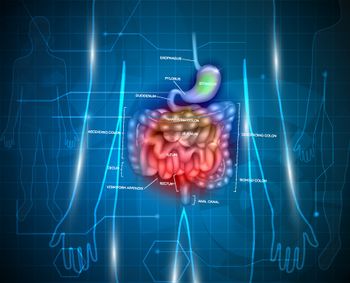
Lenvatinib is a potent multi-kinase inhibitor, with activity against several targets and the potential to reverse resistance to antiangiogenic agents. The new study included a total of 111 patients, divided into two cohorts; cohort A included 55 patients with advanced/metastatic pancreatic NETs after progression on a previous targeted agent; cohort B included 56 patients with advanced/metastatic NETs of the gastrointestinal tract after progression on somatostatin analogs.
In cohort A, 56% of the patients were female, the median age was 58 years, and the mean Ki-67 index was 9.24%. In cohort B, 41% were female, the median age was 61 years, and the mean Ki-67 index was 5.73%. Approximately half of both cohorts had had prior surgery of the primary tumor.
In the full study comprising both cohorts, there was a 29.2% partial response (PR) rate, and 66% had stable disease; 2% had progressive disease. In cohort A, the pancreatic NETs patients had a 40.4% PR rate, and 55.8% had stable disease. In cohort B, lenvatinib appeared somewhat less effective, with a PR rate of 18.5%, while 76% had stable disease.
After a median of 11 months of follow-up, the median progression-free survival (PFS) was 14.2 months in cohort A and 17.6 months in cohort B.
Most patients in both groups required dose reductions or interruptions (88.6% in cohort A, 91.1% in cohort B). Most adverse events were grade 1 or 2, with 8.6% of patients in cohort A and 9.6% in cohort B reporting a grade 3 event. There was one grade 5 adverse event in cohort A. The most frequent adverse event of any grade was fatigue, followed by gastrointestinal effects.
“Lenvatinib showed the highest response rate by central radiology assessment with a targeted agent in advanced NETs,” Capdevila said, adding that biomarker studies are currently ongoing.
Eric Baudin, MD, PhD, of Gustave Roussy Cancer Center in Villejuif, France, discussed the study for ESMO, and he highlighted that this was indeed the highest published response rate in this setting for a targeted agent. “It translated not into the highest median PFS,” he said, “but into a median PFS in the upper range of previous TKI trials.”
Baudin did note that the rates of dose interruption and dose reduction were considerable, so the tolerance of the agent may be an issue. He also said that the apparent efficacy of lenvatinib now raises a number of new questions of exactly where it fits in the treatment landscape for advanced NETs. For example, could lenvatinib challenge chemotherapy as the optimal first-line therapy in aggressive pancreatic NETs? The issue of sequencing of agents is also one that requires further study, he said.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.