Benefit of Maintenance Therapy in Metastatic Urothelial Carcinoma
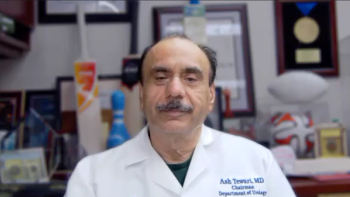
Shared insight on the broader benefits of maintenance therapy in metastatic urothelial carcinoma and the mainstay agents in this setting.
Episodes in this series

Transcript:
Petros Grivas, MD, PhD: Think about the maintenance paradigm. In my mind, there is continuation maintenance. For example, if you do EV [enfortumab vedotin] pembrolizumab, you can do continuation maintenance with pembrolizumab or both. You have the switch maintenance approach, which is the example with platinum gemcitabine with ... to avelumab maintenance. So those concepts are distinct. And of course you have a borderline resectable case. You have a borderline node-positive disease, and you potentially give chemotherapy. Do you have any case that you have, let’s say N2 [node 2], not metastasis, but N2 bladder cancer? You give, for example, Gem CIS [gemcitabine and cisplatin], you potentially go 4, 5, or 6 cycles, depending on your scenario, and you have a near CR. Would you go for a consolidative surgery or radiation in that case, or would you do maintenance avelumab in this borderline scenario?
Cora Sternberg, MD, FACP: It’s a very good question. I think it’s very important that you said 6 cycles, because I think it’s wrong when people just give 3 cycles when they have nodal disease, and they think that they’re doing neoadjuvant therapy. I think after 3 cycles another CT scan should be done. They should be evaluated, and they should continue for at least 6 cycles. In the old days with MVAC [methotrexate, vinblastine, doxorubicin, cisplatin], we gave even up to 12 cycles. We were so excited to see patients responding. And the patients who did the best then were the patients not necessarily with 12 cycles, but to whom we were able to give chemotherapy. And then we did surgery afterward. And these, we converted the partial responders into complete responders. I don’t know that that’s done as much today, and today I think we would have to discuss it in a multidisciplinary tumor board and decide whether or not we wanted to continue with avelumab maintenance in patients who have responded well or consider surgery.
Petros Grivas, MD, PhD: Absolutely. It’s a great tumor board case, right Srikala?
Srikala Sridhar, MD, MSc, FRCPC: I think it’s a great case, and we’ve faced this as well. I work really closely with my urologists and my radiation oncologist. And to your point, I would certainly present it at rounds and see what people think. It’s a good question. We’re getting the sense from the adjuvant nivo [nivolumab] data that bringing the immunotherapy earlier may be good, sequencing chemotherapy and then immunotherapy may be good. At the same time, though, I think we do need to think about local disease because local progression is really difficult. I think that we probably need a clinical trial to answer that specific question.
Petros Grivas, MD, PhD: And there is an interesting trial that comes to my mind, the INSPIRE trial, ECOG-ACRIN Cancer Research Group EA8185 (NCT04216290) by Dr. Monika Joshi. And she’s doing things a little bit differently. We have induction chemotherapy first, and then they are doing chemotherapy radiation with or without nivolumab. It’s an interesting concept going through the focus groups right now. But I agree with you, it’s a great tumor board case. Think about maintenance therapy, and Tian, we’ll ask you next, any potential biomarkers that make you think more about giving maintenance, or you would give it to anybody as long as they have a response or stable disease to platinum-based chemotherapy.
Tian Zhang, MD, MHS: The JAVELIN Bladder 100 trial (NCT02603432) really was across the population, so I don’t specifically tease out a subset of patients. I think they all should be offered maintenance avelumab after their course of chemotherapy is done, as long as they have stable disease or better. And when I think about bladder cancer in general, that predisposes us well to this maintenance treatment is that, when bladder cancer progresses, it is quite aggressive. And we all have patients who progress through and have a visceral crisis where they cannot get into any further lines of treatment. That patient population, we’re catching them, we’re seeing them quickly through the maintenance treatments, and as they become symptomatic or as they have their restaging scans, we’re catching progression earlier, hopefully, at least in my mind. And then they can see other effective strategies in the later-line settings. So hopefully we’re not getting into visceral crises so much and able to salvage disease.
There are a couple of really interesting biomarkers, certainly, for the benefit of PD-L1 inhibitors with avelumab and high PD-L1 positivity, TMB [tumor mutational burden] status that is high, although, in bladder cancer, it’s generally TMBs are on the lower side, right? Then the immunogenicity of bladder cancer, I think, still has a lot more questions than answers. In this ESMO congress forum, we’ve actually seen Dr. Thomas Powles present some interesting biomarkers from the JAVELIN study showing us that some chromatin folding with the ... expression potentially could predict some responses. Not ready for prime-time clinical use yet, but certainly really interesting data.
Petros Grivas, MD, PhD: And I’m very excited to see this biomarker program continue despite that it does not affect clinical practice. We give available maintenance regardless of molecular biomarkers based on a response or stable disease as long as there’s no counterindication to immunotherapy, we give available maintenance. But it’s nice to see the biomarker exploration program. And Cora, the question for you is, how successful do you think this maintenance program is in delaying progression and prolonging survival? The data is pretty clean. Any comments?
Cora Sternberg, MD, FACP: I think it’s extremely successful. Patients with a CR is the only one I may have a question about, but I don’t know how many CRs we really see because I don’t know if they really are CRs. But I never saw patients who had partial responders not recur, OK? And patients with stable diseases, I never saw them not recur. So, for sure, I think giving to CR and PR and stable disease patients we are definitely delaying recurrence. And I think that that’s extremely important. And when it was first published, the data, I think the hazard ratio was 0.69 and the data are holding up with time, and it’s really quite interesting. But in the past, the patients, if they had just a PR and you left them alone would always recur. I think it’s important what we’re doing.
Petros Grivas, MD, PhD: I totally agree with you. And the analysis that was done on patients with CR, PR, or stable disease, they all appeared to have benefit. And the medium patients, even with CR in the study, were short. I’m totally with you that all those patients benefit.
Transcript edited for clarity.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.