Clinical Scenario 1: A 73-Year-Old Man With Metastatic Urothelial Carcinoma
The panel reviews a clinical scenario of metastatic urothelial carcinoma where the patient is not eligible for cisplatin treatment.
Episodes in this series

Transcript:
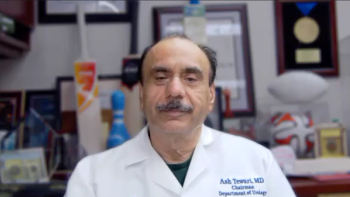
Petros Grivas, MD, PhD: I have a second case for you, and I’m going to briefly discuss it. It’s a little different from the previous scenario. A 73-year-old gentleman has hematuria. A CT scan showed a 3.4-cm tumor in the bladder. Sadly, there were lung metastases. He had an ECOG PS [performance status] 1 with no significant neuropathy, but this patient has hearing aids with grade 3 hearing loss. The creatinine clearance is 40 mL/min, which is definitely lower than 60 mL/min. It makes you wonder if this patient is going to get cisplatin with grade 3 hearing loss and a creatinine clearance of 40 mL/min. PD-L1 CPS [combined positive score] is 10. Genomic sequencing, which we do with all patients with that disease, showed that there was no mutation or fusion in FGFR2 or FGFR3. Cora, any comments on how you’d manage this patient.
Cora Sternberg, MD, FACP: I give cisplatin more liberally perhaps than in the Matthew Galsky criteria. But this patient has a creatinine clearance of 40 mL/min, so I wouldn’t give it to him. He also has hearing loss, so he has at least 2 reasons why he would be cisplatin ineligible.
This patient has 2 options. You could start with gemcitabine-carboplatin followed by avelumab maintenance. If you think that he couldn’t tolerate chemotherapy, the other option is to give him immunotherapy with pembrolizumab or atezolizumab up front. He’s not eligible for erdafitinib because he doesn’t have an FGFR mutation.
Petros Grivas, MD, PhD: Would that change if the patient had an FGFR mutation? Would you do exactly the same thing in the frontline setting?
Cora Sternberg, MD, FACP: I wouldn’t give erdafitinib in the frontline setting in any case.
Petros Grivas, MD, PhD: I totally agree. We don’t have enough data. Carboplatin-gemcitabine followed by avelumab maintenance is a very reasonable strategy.
Srikala Sridhar, MD, MSc, FRCPC: I completely agree. The only other thing I was going to mention is that sometimes it’s helpful to get your urologist or nephrologist involved because that kidney function may be a function of obstruction. There may be a way to improve kidney function before starting chemotherapy. It may allow patients to get gemcitabine-carboplatin, for example, when you think they can’t. I agree. I’d give gemcitabine-carboplatin in this setting. We don’t have the approval of frontline I/O [immuno-oncology], so more people get gemcitabine-carboplatin—which isn’t a bad thing—followed by something like avelumab.
Cora Sternberg, MD, FACP: It’s very important to make sure patients don’t have hydronephrosis and don’t need to have stenting or percutaneous nephrostomy. But this patient does have hearing loss, and I don’t think they can fix that as easily. I don’t think it’s a patient for cisplatin in any case. I agree with working with the urologist closely to evaluate it.
Petros Grivas, MD, PhD: That’s a great point. If you take the hearing loss away, if someone has an obstruction with hydronephrosis, can you put in a nephrostomy tube to compress the kidney, optimize the GFR [glomerular filtration rate], and potentially give cisplatin in that different scenario? Even in the neoadjuvant setting, I prefer a nephrostomy tube vs a stent because there’s a very small risk of upper-tract seeding with stents in localized disease settings. I use nephrostomy tubes to optimize kidney function in the neoadjuvant setting as well.
Transcript edited for clarity.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.