- ONCOLOGY® Companion, Volume 38, Supplement 2
- Volume 38
- Issue 02
- Pages: 15-17
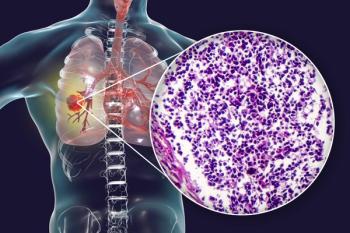
Experts Examine the Need for Targeted Therapy Options for KRAS G12C–Mutated NSCLC
Narjust Florez, MD, and Sandip P. Patel, MD, cohosted a X chat centering on treatment options for KRAS G12C non–small cell lung cancer.
Narjust Florez, MD, and Sandip P. Patel, MD, cohosted a X chat, formerly known as Twitter, centering on treatment options for KRAS G12C non–small cell lung cancer (NSCLC), with a specific focus on hepatotoxicity and brain metastases. To start the chat, they reviewed a patient case of a 63-year-old woman who presented with dyspnea and fatigue. The experts then discussed how they would best treat this patient as well as treatment options for those with KRAS G12C NSCLC. Florez, associate director of the Cancer Care Equity Program and thoracic medical oncologist at the Dana-Farber Cancer Center in Boston, Massachusetts, and Patel, professor of medicine at University of California San Diego Health, also looked at recent updates to the National Comprehensive Cancer Network (NCCN) guidelines and results from the phase 1/2 KRYSTAL-1 trial (NCT03785249).1
To begin the discussion, Florez gave a brief case overview. She stated that the treatment was appropriate in this setting and that the patient should respond to immunotherapy. Patel highlighted the NCCN guidelines, stating, “For KRAS G12C–mutated [metastatic] NSCLC, the initial treatment is chemoimmunotherapy. Second-line treatment options include KRAS G12C mutation–specific small molecular inhibitors such as sotorasib [Lumakras], adagrasib, or docetaxel-based chemotherapy.”2
Florez noted the importance of biomarker testing for patients with cancer. In response to Florez asking Patel about whom he prioritizes for biomarker testing, he responded that he prioritizes any patient with nonsquamous metastatic NSCLC independent of smoking history. Molecular testing helps Patel to “find the targeted therapy option for my patients but also avoid improper use of [immunotherapy].”
As Patel alluded to picking tailored therapy options, Florez cited results from a JAMA Network study that found patients who had mutations and received tailored therapy had an 18.6-month improvement in overall survival (OS) vs 11.4 months in patients who did not (P <.001).3 The conversation then switched to the updated efficacy results from the KRYSTAL-1 trial. This trial used adagrasib for patients with KRAS G12C NSCLC. The data that were presented by Patel during the chat showed a positive efficacy benefit for the adagrasib arm.
Central nervous system (CNS) activity was observed during the KRYSTAL-1 study. Florez said that patient comorbidities and previous adverse effects (AEs) from other therapies should be considered. Grade 3 treatment-related AEs (TRAEs) occurred in 40.9% of patients. Additionally, 3% of patients had grade 4 TRAEs and 2.3% had grade 5 TRAEs. For 1 patient each, the grade 5 TRAEs included pneumonitis, cardiac failure, and pulmonary hemorrhage.
A dose reduction occurred in 51.5% of patients, and 9.1% discontinued treatment. For 1 year or more, 32.6% of patients were given adagrasib.
For targeted therapy, medical reconciliation is key to achieving positive results. Florez also offered the use of sotorasib as a good alternative to adagrasib. The use of proton pump inhibitors and H2 antagonists should be “used with caution with sotorasib” because the drug absorption may be decreased.
According to Patel, hepatotoxicity is important to be managed with KRAS G12C inhibitors. In previous trials, toxicity has been observed when there is proximity to immunotherapy. Clinicians can manage this by stopping therapy and resuming at a lower dose once the patient has recovered.
Regarding AE management, communication between clinicians, the patient, and the entire care team is key. Florez typically sees AE presentation within 2 to 4 weeks of beginning treatment.
Regarding the KRYSTAL-1 study, an analysis of intracranial efficacy was conducted.4 Patel emphasized the need for close collaboration between medical oncologists, radiation oncologists, and neuro-oncologists.
The analysis included 25 patients who had received adagrasib in the KRYSTAL-1 trial and developed CNS metastases. The intracranial overall response rate was 42%, and the disease control rate was 90%. Additionally, the median progression-free survival was 5.4 months and the median OS was 11.4 months.
Looking at the final part of the patient case, Florez and Patel were asked what they would do if this patient presented again with additional lung tumors and adrenal metastases. “My No. 1 choice is to consider a clinical trial; many KRAS inhibitors are currently under development, some with promising activity. If a clinical trial [is not an] option, we could consider docetaxel or single-agent chemotherapy,” Florez said.
Patel agreed with her treatment prerogatives. He added that he also considers palliative care or stereotactic body radiation therapy. Florez seconded his opinion and tagged radiation oncologists to hear their thoughts.
Matthew Katz, MD (@subatomicdoc), responded to the tag by saying, “I usually ask for some guidance because the patterns of progression vary. Symptomatic oligoprogression is an easier decision than for radiologic only. Also have to know when it may be the start of multifocal progression.”
Drew Moghanaki, MD (@DrewMoghanaki), also responded, stating, “It depends on the volume of tissue to be targeted and assurance that the patient doesn’t already have runaway disease. If both issues are not concerning, then the risk-to-benefit ratio will be in favor of [local consolidation therapy].”
Moving forward, Patel believes that combination therapy should target escape pathways for patients with KRAS G12C NSCLC. However, molecular testing should continue to be encouraged prior to beginning treatment and should be retained across all subsequent therapies.
For Florez, this is just the beginning of studying KRAS G12C. Combination treatments are under investigation, and toxicity is always being evaluated.
To date, there have been no cross-comparison trials, which could be beneficial in the future. Florez is hopeful that as more data are presented, they can use them to help target treatments for patients with KRAS G12C NSCLC.
References
- Mirati presents two-year follow-up data from KRYSTAL-1 study demonstrating durable response and long-term overall survival at 2023 World Conference on Lung Cancer. News release. Mirati Therapeutics. September 9, 2023. Accessed January 11, 2024.
https://prn.to/3Sf905G - NCCN. Clinical Practice Guidelines in Oncology. Non–small cell lung cancer, version 1.2024. Accessed January 11, 2024. https://bit.ly/48zaLAr
- Singal G, Miller PG, Agarwala V, et al. Association of patient characteristics and tumor genomics with clinical outcomes among patients with non-small cell lung cancer using a clinicogenomic database. JAMA. 2019;321(14):1391-1399. doi:10.1001/jama.2019.3241
- Negrao MV, Spira AI, Heist RS, et al. Intracranial efficacy of adagrasib in patients from the KRYSTAL-1 trial with KRASG12C-mutated non-small-cell lung cancer who have untreated CNS metastases. J Clin Oncol. 2023;41(28):4472-4477. doi:10.1200/JCO.23.00046
Articles in this issue
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.