
A subgroup analysis of the phase III RECOURSE trial has shown that TAS-102 is effective at improving survival in patients with both KRAS wild-type or mutant metastatic colorectal cancer.

Your AI-Trained Oncology Knowledge Connection!


A subgroup analysis of the phase III RECOURSE trial has shown that TAS-102 is effective at improving survival in patients with both KRAS wild-type or mutant metastatic colorectal cancer.

Two phase III trials have confirmed the benefit of regorafenib, an oral multikinase inhibitor, in patients with previously treated metastatic colorectal cancer.

Large proportions of lung and colorectal cancer patients believe that surgery will cure their cancer, according to results of a new population-based study.

Adding the oral NK1 antagonist aprepitant to an oxaliplatin-based chemotherapy regimen effectively reduced nausea and vomiting in colorectal cancer patients.

A new study has found that in patients diagnosed with metastatic colorectal cancer, a low BMI could be a poor prognostic factor.

The FDA has granted a priority review for MM-398 as a second-line treatment for metastatic pancreatic cancer after the drug demonstrated improved survival.

Ahead of the ESMO World Congress on Gastrointestinal Cancer, we are discussing the use of maintenance therapy in metastatic colorectal cancer with Axel Grothey, MD.

Researchers have discovered a protein encoded by the GPC1 gene present on cancer exomes that may be used as a diagnostic tool to detect early pancreatic cancer.

Patients with treatment-naive metastatic pancreatic cancer assigned to treatment with gemcitabine plus rigosertib did not have any improvement in tumor response or survival compared with treatment with gemcitabine alone.

The presence of an abdominal blood clot may be a sign of cancer and may also be associated with poor survival for patients with pancreatic or liver cancers.

In this video, Dr. El-Khoueiry discusses results from a phase I/II study that suggest the PD-1 inhibitor nivolumab is safe and effective in advanced hepatocellular carcinoma.

In this video, Dr. Atsushi Ohtsu discusses the use of TAS-102, an oral combination of trifluridine and tipiracil hydrochloride, in refractory colorectal cancer.

Aspirin use after a colorectal cancer diagnosis was independently associated with improved rates of both cancer-specific and overall survival.

Treating patients with unresectable colorectal liver metastases with radiofrequency ablation and chemotherapy resulted in improved long-term overall survival.

Neoadjuvant mFOLFOX6 plus radiation improved pathologic complete response in advanced rectal cancer patients compared with 5-FU/radiation or mFOLFOX6 alone.

In this video, Dung T. Le, MD, discusses a phase II study that found that mismatch repair–deficient colorectal tumors were highly responsive to checkpoint blockade with the anti–PD-1 drug pembrolizumab.

Increased levels of vitamin D were associated with improved overall survival rates in metastatic colorectal cancer patients treated as part of CALGB/SWOG 80405.

Results from a phase I/II study suggest that the immunotherapy nivolumab is safe and effective in advanced hepatocellular carcinoma (HCC).

Aflatoxin, a naturally occurring toxin produced by certain types of molds, has been found to be associated with an increased risk of gallbladder cancer.

Colorectal tumors that lacked the ability to repair DNA were found to be highly responsive to checkpoint blockade with the anti–PD-1 drug pembrolizumab.

Ahead of the 2015 ASCO Annual Meeting, we are discussing over-the-counter therapies for patients with metastatic colorectal cancer with Andrew T. Chan, MD, MPH.

The CONCUR trial found that regorafenib improved overall survival in a large group of Asian patients with treatment-refractory metastatic colorectal cancer.
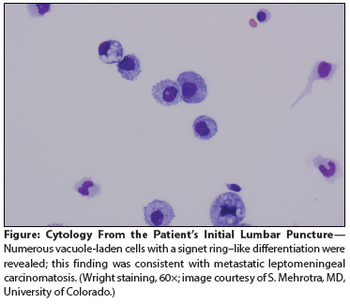
A 59-year-old man with metastatic gastric cancer presented to the oncology clinic with a 1-week history of positional headache, nausea, and vomiting. He stated that the headache was located in the frontal region, was 8 on a scale of 10 in intensity.

TAS-102, an oral combination of trifluridine and tipiracil hydrochloride, improved median overall survival in patients with refractory colorectal cancer.

Metformin, a common drug for type II diabetes, did not improve the survival of patients with pancreatic ductal adenocarcinoma.