Oral JAK2 inhibitor deflates symptoms in myelofibrosis disease
NEW ORLEANS-A new treatment for patients who are severely debilitated by myelofibrosis offers hope of a return to normal daily life. Preliminary studies with an oral drug INCB018424 that targets the Janus-activated kinase (JAK) 2 gene appears to markedly reduce the swelling of the spleen and sometimes the liver, which can, in turn, can change patients’ quality of life.
NEW ORLEANS-A new treatment for patients who are severely debilitated by myelofibrosis offers hope of a return to normal daily life. Preliminary studies with an oral drug INCB018424 that targets the Janus-activated kinase (JAK) 2 gene appears to markedly reduce the swelling of the spleen and sometimes the liver, which can, in turn, can change patients’ quality of life.
“The results have been quite amazing in terms of benefit to the patient,” said Srdan Verstovsek, MD, PhD, associate professor in the department of leukemia at M.D. Anderson Cancer Center in Houston. “More than 75% of the patients are still in the study after an average of 16 months.” The ability for patients to remain on treatment long-term indicates that treatment is safe as well as effective, added Dr. Verstovsek speaking at an ASH 2009 press conference.
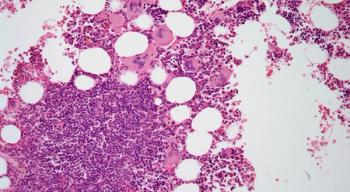
Dr. Verstovsek explained that uncontrolled growth of bone marrow cells elicits a cytokine reaction which, in turn, creates an inflammatory response causing fibrosis and scarring. Because the bone marrow cannot produce enough blood cells, the body puts greater demand on the spleen and liver to produce the cells, leading to splenomegaly.
“Because of that, patients have very poor quality of life. They suffer from a lot of side effects, including body wasting, pruritus, and night sweats, and they usually die between five and seven years after diagnosis,” Dr. Verstovsek said.
His group enrolled 155 patients with either primary myelofibrosis or myelofibrosis occurring after polycythemia vera or essential thrombocythemia. He said the study was the largest ever performed for the disease.
Patients received an individually optimized dose of 10 mg, 15 mg, or 25 mg of INCB018424 twice a day. Efficacy of INCB018424 was assessed by measuring the spleen with MRI at one, three, and six months. Patients also were surveyed about the impact of the treatment on their health and well-being. The impact of INCB018424 on exercise capacity was measured with a standardized six-minute walk test (
Dr. Verstovsek said the treatment benefit was seen primarily in the significant and rapid reduction in splenomegaly in these patients. Half of the patients have experienced a reduction of their spleen volume by at least 50% as determined by palpation.
He said patients also appear to have a reduction in or an elimination of symptoms of pruritus, night sweats, abdominal discomfort, bone pain, and fatigue. “They stop their weight loss and gain weight and actually can walk more. They start to enjoy their life and have a normal quality of life again,” he said.
Finally, treatment with INCB018424 also resulted in improvements in the six-minute walk test, with median increases from baselines of 33, 58, and 70 meters after one, three, and six months of therapy, respectively.
“There are no approved therapies for this disease,” Dr. Verstovsek said. The development of INCB018424 followed the late 2004 discovery of a mutation in the JAK2 gene that was observed in about 50% of the patients with myelofibrosis. The mutated gene creates a protein that contributes to uncontrolled cell growth.
Commenting on the study was Richard Larson, MD, professor of medicine at the University of Chicago, who noted that “our measurements of response are usually quite objective, such as improved blood counts and prolongation of survival. Measuring improvements in symptoms has been more difficult.”
Dr. Verstovsek said that because the drug inhibits the normal JAK2 “we do see, in some patients, a lowering of the blood count and low platelet counts. This can be avoided very nicely by selectively targeting the dose in each patient to avoid myelosuppression and still provide full benefit.”
He said that by optimizing the dosing schedules, incidents of anemia and thrombocytopenia are less than 5%. Phase III studies in the U.S., Canada, and Australia as well as in Europe are under way.
Omacetaxine targets imatinib-resistant CML
In another study, the investigational drug omacetaxine allowed patients with chronic myeloid leukemia (CML) to achieve complete cytogenetic responses despite the fact that the patients carried the T315I-positve mutation, making their disease resistant to imatinib (Gleevec).
Jorge Cortes-Franco, MD, deputy chair of the department of leukemia at M.D. Anderson Cancer Center, said that 86% of patients were able to achieve a complete hematologic response when treated with the subcutaneously administered omacetaxine. He said 18% of those patients had complete cytogenetic responses (
Genes and ALL
Researchers from the Children’s Hospital of Philadelphia (CHOP) set out to find out why 221 infants with acute lymphoblastic leukemia (ALL) responded poorly to chemotherapy.
“MLL translocations are the most pervasive molecular abnormalities in infant ALL and are poor prognostic factors; however, interrelationships between specific MLL partner genes, event-free survival (EFS), and clinical covariates have been elusive due to several factors,” wrote the researchers from the Children’s Oncology Group (COG) P9407 trial (
For this trial, MLL status was defined by several methods, including karyotype; reverse transcriptase polymerase chain reaction (RT-PCR) analysis of MLL translocations with AF4, ENL or AF9; and cDNA or genomic panhandle PCR. Kaplan-Meier plots were used to estimate EFS as a function of MLL status, MLL partner gene and, within MLL status and partner gene subsets, as a function of age at diagnosis, the authors wrote. MLL status was determined in 210 of 221 total cases.
According to the results, 74% of infants had an MLL translocation and the most common partner genes of MLL were AF4, ENL, and AF9, said lead author Blaine Robinson, PhD. “MLL translocations, young age, and high white blood cell counts have correlated with poor outcome in infant ALL before, but this MLL classifier in the largest cohort of infant ALL with detailed molecular characterization reported to date adds new elements to the impact of MLL partner genes on outcome and their connection to prognostic factors. AF4 and ENL not only negatively impact EFS, but this effect is larger in the younger infants,” the researchers wrote.
“The ability to characterize acute lymphoblastic leukemia based on specific partner genes may provide a new way to determine whether infants with ALL, in which the partner genes of MLL are different, will benefit from specific types of treatment,” said senior study author Carolyn A. Felix, MD, professor of pediatrics at CHOP.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.