
Incorporating MRI-based parameters into a risk model could cut down on the number of unnecessary biopsies performed in patients with suspected prostate cancer.

Your AI-Trained Oncology Knowledge Connection!


Incorporating MRI-based parameters into a risk model could cut down on the number of unnecessary biopsies performed in patients with suspected prostate cancer.

The observed narrowing of racial disparities in prostate cancer outcome since the advent of PSA screening is not as large as previously believed.

The approval of the oral androgen-receptor inhibitor apalutamide (Erleada) is the first to be based on metastasis-free survival.

Researchers reported promising safety data from an ongoing phase Ib/II clinical trial for SM-88, an investigational combination therapy that might one day offer an alternative to androgen deprivation therapy for men with recurrent, nonmetastatic prostate cancer.

Enzalutamide resulted in a 71% reduction in metastatic disease risk among men with castration-resistant prostate cancer and rapid prostate-specific antigen doubling time, according to the first interim analysis of data from the phase III PROSPER trial.

Researchers are developing a prognostic hypoxia gene signature for patients with localized prostate cancer that could predict biochemical failure and metastasis.

The US Food and Drug Administration has approved abiraterone acetate (Zytiga) tablets in combination with prednisone for the treatment of metastatic prostate cancer patients with high-risk, castration-sensitive disease.

Adding docetaxel chemotherapy to frontline hormone therapy improves quality of life and may reduce the need for subsequent treatment, according to an analysis from the STAMPEDE trial.

Apalutamide was well-tolerated and associated with delayed metastasis in men with high-risk castration-resistant prostate cancer that has become refractory to conventional hormone therapy, according to an early interim analysis of the phase III SPARTAN clinical trial.

Adjuvant radiotherapy after prostatectomy resulted in lower rates of biochemical recurrence, distant metastases, and death compared with surveillance followed by early-salvage radiotherapy in patients with high-risk prostate cancer, according to a new study.

Long-term follow-up of a large phase III study showed that chemohormonal therapy involving docetaxel added to androgen deprivation therapy (ADT) prolongs overall survival over ADT alone in metastatic hormone-sensitive prostate cancer patients with high-volume disease.

The time to testosterone rebound was associated with differences in prostate cancer–specific and cardiovascular mortality among men who underwent RT and ADT.

Adding abiraterone plus prednisone to ADT improves patient-reported outcomes and quality of life in patients with metastatic castration-naive prostate cancer.

Educational strategies including pamphlets and recommendations from family physicians and support from a specialist can improve bone care in men with prostate cancer undergoing androgen deprivation therapy.

The use of bipolar androgen therapy was safe and resulted in responses to enzalutamide in metastatic castration-resistant prostate cancer patients after initial therapy.
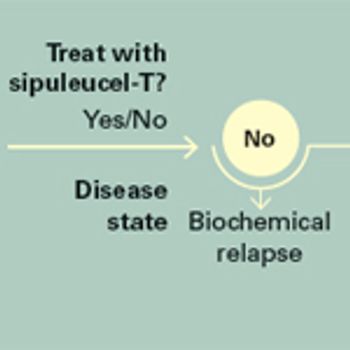
Multiple immunotherapy platforms have been investigated for prostate cancer, but sipuleucel-T still remains the sole approved autologous cellular immune product that can be used in men with asymptomatic or minimally symptomatic metastatic castration-resistant prostate cancer.

A novel classification system that incorporates genomic risk with clinical variables was able to accurately identify prostate cancer patients at low, intermediate, and high risk for metastasis.

In this review, we will examine the theories supporting treatment to achieve local disease control in oligometastatic prostate cancer, analyze the evidence supporting cytoreductive prostatectomy, and review selected relevant ongoing clinical trials.
Quality of life is better after modern radiotherapy compared with surgery.

Most men with clinically important localized prostate cancer deserve first-line open or robotic radical prostatectomy.

Men with Medicaid are more likely to present with metastatic prostate cancer than men presenting with prostate cancer who have private insurance, according to a new study. There are racial disparities in terms of prostate cancer outcomes among those privately insured, but not among Medicaid recipients.

In this interview we discuss the STOPCaP trial, a meta-analysis that looked at optimal systemic therapy options for men with metastatic hormone-sensitive prostate cancer.

Serial PSA testing with early salvage radiotherapy is a viable option in most high-risk men.
The data for adjuvant radiotherapy remain strong.

This video reviews 4-year quality-of-life results from a prospective, population-based study that looked at prostate cancer patients who selected either active surveillance, radical prostatectomy, or external-beam radiation.