Leukemia
Latest News

Latest Videos

CME Content
More News
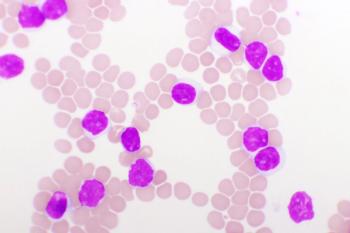
In a population of patients with chronic myeloid leukemia with resistant disease experienced promising activity following treatment with ponatinib regardless of T315I mutation status.

High rates of undetectable minimal residual disease were found in fit patients with chronic lymphocytic leukemia who were treated with venetoclax plus either obinutuzumab or ibrutinib vs chemoimmunotherapy.
Ibrutinib and ventoclex given in the frontline setting demonstrated deeper and longer minimal residual disease for elderly and unfit patients with chronic lymphocytic leukemia.
Patients with chronic lymphocytic leukemia who were treated with ibrutinib and venetoclax in the first line continued to demonstrate deep, durable responses with new data showing further benefit to continuous ibrutinib therapy after 2 years.
The combination of MRD-guided ibrutinib and venetoclax demonstrated feasibility for treating patients with relapsed/refractory chronic lymphocytic leukemia.

The FDA has approved rituximab plus chemotherapy for previously untreated pediatric CD20-postive diffuse large B-cell lymphoma, Burkitt lymphoma, Burkitt-like lymphoma, and mature B-cell acute leukemia following results from the phase 3 Inter-B-NHL Ritux 2010 study.
Patients with chronic lymphocytic leukemia or small lymphocytic leukemia treated with zanubrutinib, obinutuzumab, and venetoclax experienced increased rates of undetectable minimal residual disease in peripheral blood and bone marrow.
DNA Sequencing of Bone Marrow Is Predictive of ALL Relapse Following Treatment With Tisagenlecleucel
DNA sequencing to detect minimal residual disease and eventual relapse was more accurate than flow cytometry for adult and pediatric patients with acute lymphoblastic leukemia who have been treated with tisagenlecleucel.
Pediatric patients with KMT2A-rearranged acute myeloid leukemia who were treated with gemtuzumab ozogamicin plus standard chemotherapy experienced improved event-free survival and a reduced relapsed risk.
Patients with relapsed chronic lymphocytic leukemia who were treated with either limited or continuous venetoclax and rituximab experienced improved responses during a 5-year follow-up.
Investigators announced positive topline results for the phase 3 QuANTUM-First trial, assessing the use of quizartinib plus chemotherapy for adult patients with newly diagnosed FLT3-ITD–positive acute myeloid leukemia.

Patients with relapsed/refractory adult B-cell acute lymphoblastic leukemia who were treated with AUTO1 experienced durable responses.

“I’ve done a lot of work [not only with] clinical trials, but also understanding the disease, the prognostic factors, and the management of adverse effects.”
Patients with mutant-IDH2 acute myeloid leukemia experienced a better overall response rate when treated with enasidenib plus azacitidine compared with azacitidine alone.
A phase 1b/2 trial found that the combination of enasidenib plus azacytidine improved overall responses and was well tolerated compared with azacytidine monotherapy for patients with newly diagnosed, mutant-IDH2 acute myeloid leukemia.

A phase 2 study found that acalabrutinib monotherapy followed by treatment with venetoclax and obinutuzumab in the frontline setting was highly active and tolerable for patients with previously untreated chronic lymphocytic leukemia despite not meeting the primary end point.

The FDA granted accelerated approval to asciminib for the treatment of patients with Philadelphia chromosome–positive chronic myeloid leukemia for 2 indications.

ASTCT recently published an article in their journal Nucleus detailing CAR T therapy in patients with acute lymphoblastic leukemia.
In a debate, experts discuss the importance of IGHV and TP53 mutational status in predicting response to novel therapies in chronic lymphocytic leukemia.
Ibrutinib for treating patients with chronic lymphocytic leukemia increased the risk of atrial fibrillation, bleeding, and heart failure in results of a cohort study.
Patients with chemotherapy-refractory, high-risk acute myeloid leukemia achieved promising benefit from treatment with ficlatuzumab and cytarabine.
Adding venetoclax to cladribine, high-dose cytarabine, and idarubicin appears to yield high rates of minimal residual disease negativity and promising survival in patients with newly diagnosed acute myeloid leukemia and high-risk myelodysplastic syndrome.

The FDA has approved the use of CD19-directed CAR T-cell therapy brexucabtagene autoleucel for adult patients with relapsed/refractory precursor acute lymphoblastic leukemia.

A recently published article on CAR T cells in patients with acute myeloid leukemia is featured by CancerNetwork's Strategic Alliance Partner ASTCT.
As more novel therapeutic targets are discovered in patients with chronic lymphocytic leukemia, the more possibilities are presented in terms of treatment with targeted agents, small molecules, and cellular therapies.